Root canals have become ubiquitous with over 22 million performed each year in the United States alone, according to the American Association of Endodontics. “You need a root canal”, is now almost as common as hearing you need a filling. It is a sales tool that is used by the dental profession because people do not want to lose their teeth. It is the only treatment protocol available to retain a tooth that is diseased. Yet, just how safe are root canals? What does scientific research say about root canal treatments? These questions are not new, nor are the findings.
- Over a hundred years ago, Dr. William Hunter was investigating the relationship between dental diseases and systemic diseases. Dr. Frank Billings, described a focal infection as “a circumscribed area of tissue infected with pathogenic organisms.” It was during this time that the term “Focal Infection Theory” was born.
- Dr. Edwin Rosenow followed Billings and discussed dental infections, particularly in multirooted teeth, where there was evidence of infection of the pulp, even with asymptomatic teeth. He noted that these teeth may be the source of systemic diseases and may need to be removed. He stated the root canal procedures should cease.
- Next came Dr. Weston A. Price, whose ground-breaking work on root canal research was and is one of the most important discoveries in the past 100 years related to health and systemic disease.
Dr. Weston Price was head of research for the dental association for 14 years during the 1920s and 30s. He published the results of 1000 extracted teeth in which canal sterilization was done in the dental research laboratory. Price led his team of 60 of the most important scientists of the day, including Charles Mayo, Victor Vaughn, Milton Rosenau, and many others, were the founders of investigating dental disease and whole-body health. Researchers in the laboratory used not just the routine sterilizing chemicals, but extremely potent sterilizing agents (more toxic than could possibly be used in the mouth) and in a highly controlled sterile environment. Their microbiology specialists found that 97 percent were cultured to find re–contamination within 48 hours. In other words, they were still there.
Price described finding bacterial growth in root canals that could be transferred into animals and create the same diseases the donor human had in from 80 to 100 percent of the animals. Heart disease, in particular, could be transferred 100 percent of the time. Many of the bacteria found were quite pathological. His research has since been suppressed by the various Dental Associations in the United States.
In the words of Dr. Weston A. Price:
- Root fillings rarely fill pulp canals sufficiently perfectly to shut out bacteria, completely or permanently.
- Root fillings usually fill the pulp canal much less perfectly sometime after the operation, due to the contraction of the root-filling material.
- The ultimate volume contraction of the root filling is approximately the amount of solvent used where a solvent is used with gutta-percha as a root-filling material.
- Infection is a relative matter, and quantity and danger are both related to defense, which defense may vary from high to exceedingly low.
- Found that root canal teeth were always infected regardless if they were symptomatic or asymptomatic.
- A considerable number of the members of the dental profession of today do not want to hear the message that condemns the teeth upon which they desire to make operations. It is necessary for this and for other reasons, including politics and the jealousies and institutional ambitions and pride, that for the greatest efficiency the institutions that will do the most fearless and aggressive dental research will be independent to function in every way that will best accomplish the attainment of new truth.
- The dentistry of the future must be fundamentally based upon a foundation of pathology rather than of mechanical skill and art. No less art and skill will be needed in the legitimate restorations, but the operation of choice will not be decided on mechanical bases.
Dr. Hal Huggins, followed the work of Dr. Weston Price, and looked at the DNA of crushed root tips. He found 83 different anaerobic bacterial species. The root canals contained 53 different species out of 8 samples. Some were more dangerous than others, and some occurred more frequently, some occasionally. Selecting those that occurred more than 5% of the time, he found:
- Capnocytophaga ochracea
- Fusobacterium nucleatum
- Gemella morbillorum
- Leptotrichia buccalis
- Porphyromonas gingivalis
In the words of Dr. Hal Huggins:
- Dentists claim they can “sterilize” the tooth before forcing the gutta percha wax down into the canal. Perhaps they can sterilize a column of air in the center of the tooth, but is that really where the problem is?
- Bacteria wandering out of the dentinal tubules is what Price was finding, and what we were finding in the crushed tooth samples.”
- “We tested blood samples adjacent to the removed teeth and analyzed them for the presence of anaerobic bacteria. Approximately 400% more bacteria were found in the blood surrounding the root canal tooth than were in the tooth itself.
- It seems that the tooth is the incubator. The periodontal ligament supplies more food, therefore higher concentration of bacteria. “
Using DNA testing technology, DNA ConneXions has identified multiple pathological bacteria found within root canal teeth, the bone adjacent to the teeth, and even more in extraction sites where healing has not taken place. This non–healing occurs in greater than 99 percent of wisdom tooth extraction sites. Additionally, large defects of non-healing are often found upon surgical exploration into the bone – about the size of the original wisdom tooth. Other sites leave what are called “cavitations” as well.
For years, comedians have poked fun at root canals and the pain associated with the procedure. Little did they know that the pain was not short lived. As mentioned above microbiology researchers during the time of Hunter, Billing, Rosenow, and Price found that bacteria and their toxins from root canals could enter the blood stream and travel to any point in the body, and generate disease to that tissue or organ. The dental association, concerned about liability issues, insisted that the nerve chamber in the center of the tooth could be effectively sterilized, and that the body would accept a root canal tooth as — not a “dead tooth” as it was previously called — but a “non-vital” tooth – a new and much more acceptable term for a root canal. Incidentally, non– vital means dead.
Even though Dr. Weston Price was one of the most decorated dental researchers of all time, he is still being ridiculed by dental leaders, even more than 70 years after his death. Many dental professionals still maintain his research is not valid. Why? Fear. For disclosing the truth about the toxicity from root canals would heap tremendous liability upon the dental association as well as individual dentists. It would also ruin a very lucrative practice in dentistry and the specialty of endodontics. The American Endodontic Association, as well as the American Dental Association (ADA), insists that they have proved Mayo’s and Dr. Price to be wrong. There is no research to support this claim, and none can be produced. Yet dentists are continually threatened with license revocation if they expose the truth about root canals or even suggest they may be dangerous.
Just as they have seen many colleagues lose their licenses for exposing the toxicity of mercury in so–called “silver” fillings, which actually contain 50 percent mercury, dentists fear for loss of their income source if they mention root canals as a source of disease.
Today, there are many diseases termed, “of unknown etiology,” which means, “we have not the first clue where they are coming from.” Many health-oriented dentists and physicians are beginning to recognize that these incurable, non–responsive diseases are showing improvements by techniques involving removal of root canal teeth and fortifying the patient’s immune system. Threats, law suits, and professional humiliation have been used against dentists who stand up for their patients, and against the ADA.
How big is the problem of root canals? In 1990, the ADA set a goal (quota) of dentists performing 30 million root canals per year in the US by the year 2000. Dentistry accomplished this by 1999.
Ask your friends. How many have root canals? How many of those friends are taking medications for some vague disease on a daily basis? Of those people treated for non–responsive diseases, perhaps as many as 90 percent have root canals.
For example, Dr. Josef Issels of Germany found that in his 40 years of treating “terminal” cancer patients, 97 percent of his cancer patients had root canals. He would not initiate his successful treatments until all root canals had been removed.
Science is showing that root canals have been found in people with Multiple sclerosis, Lou Gehrig’s disease, Lupus, leukemia, diabetes, arthritis, and a host of other autoimmune diseases. Reversal of these diseases, as shown by improvements in physical conditions as well as positive changes in blood chemistries, occur after the removal of dental toxic challenges (mercury, nickel, aluminum, root canals and cavitations) in conjunction with stimulation to the immune systems of these people. We have seen this in our patients over decades of clinical observations.
Thousands of lives are challenged daily by the placement of root canals, and when these patient’s genetic weak links break, they and their families are doomed to financial and health losses that destroy their ability to work, play, raise families and enjoy life, liberty and the pursuit of happiness.
The reason is simple. Extremely toxic anaerobic bacteria have been found and identified in and around root canals.
All reasonably informed citizens in the US understand that alcohol and tobacco potentially create health hazards. They have a choice. Citizens are not informed of the multiple disease producing bacteria living in their root canals. If people were informed of the hazards created by “anaerobic” bacteria living in the periodontal ligament surrounding these root canal teeth, they could at least make an informed choice about whether or not to risk this potentially life altering procedure.
These anaerobic bacteria have now been identified by DNA analysis of the teeth, blood adjacent to the root canal teeth, and cavitations,” or the bone defects left behind by tooth removal in which the contaminated periodontal ligament is left in place. These patients have been informed by their fear–laden, but trusted dentist, that root canals are perfectly safe. They are told that root canal teeth are “sterile.”
This simply is not true.
A protective barrier is formed around many root canal teeth that allow nutrients from the blood to enter, but prevent access of antibiotics and white blood cells of the immune system to try to heal the areas. As toxins seep out into the blood stream when the owner of the root canal bites down on food, toxins are forced into the blood with access to every location in the body that might have a weak spot. “Sterilizing the tooth” just does not happen. Yes, a column of air in the pulp chamber is cleaned, but the real problem is in the periodontal ligament that surrounds the tooth. That is the incubator in which billions of bacteria can breed.
Today’s DNA research has found not only the bacterial species that Dr. Price discovered in the ’20s, but many more that have the ability to create disease.
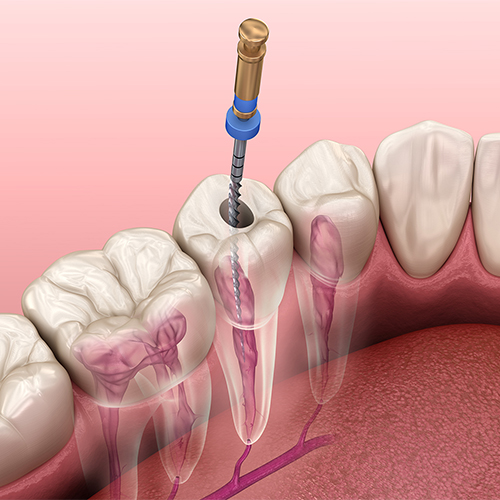
Where did these pathogens (bacteria that can cause disease) come from? They were in the dentin tubules – over three miles of tiny tubes per tooth that constitute the mid-section of the tooth called the dentin. This is located right below the enamel, and adjacent to the pulp chamber. Where do these bacteria go in real life? They travel down the tubules to the periodontal ligament which is the attachment between tooth and bone. An area impossible to sterilize, and where neither antibiotics nor white blood cells of the immune system can reach this protected location. Every time a person bites down — as in chewing — some of these bacteria — or worse yet, their toxins, are squirted into the body’s lymphatic drainage system. From here they go to the blood stream. From there — everywhere.
Why should the public be concerned? With millions of root canals out there, and thousands having been told they need one every month, the potential for problems is past epidemic almost to the endemic stage. Again, it must be pointed out, those people are not informed about the hazard they are about to have inflicted on themselves. In most cases, neither is the dentist.
Everyone who receives a root canal has an incubator in those dentinal tubules that is growing anaerobic bacteria that can create whatever disease their genetic weak link would prefer. This is no longer a one microbe, one disease, one drug to cure, world. Multiple bacteria families, joining hands with toxic metals like mercury and nickel, now endeavor to create new diseases unfamiliar a hundred years ago.
It is contended that dentists “sterilize” the dead tooth. And that is true, they do. However, no matter what the pulp chamber is embalmed with (a wax cone called gutta percha is generally placed into the canal), the tooth is still dead. The body does not accept dead structures as safe. In fact, it launches an autoimmune response against the dead tooth. This is the origin of many autoimmune diseases, compounded by the presence of pathological bacteria and their toxins.
What about these anaerobic bacteria? The ones that live in the absence of oxygen? Who are they, and in which patients are they found?
Dr. Huggins stated the following: “Our observations over the past 40 years suggest that the old theory of one microbe — like Strep pneumonia — gives one disease, like pneumonia, that is cured by one drug – penicillin, is being replaced by group warfare. Toxic dental metals are known to alter the integrity of the cell membrane, called cell membrane permeability. Reduction of quality allows weaker bacteria to invade the cells, but once inside the membrane, even a weak bacterium and cause lethal results to the cell.
“Bacterial invasion is not consistent. If we identify the bacteria of several root canals in a person with Multiple sclerosis (MS) or Lou Gehrig’s disease (ALS) with DNA technology, we do not find the identical bacteria in each dead tooth.
“For instance, in root canals or cavitations in people with MS, a bacterium, Enterobacter was found. It was also found in ALS and Alzheimer patients (AD). Is there a similarity, since they are all neurological diseases? Enterobacter is noted for involvement in endocarditis (inflammation around the heart), bone infections — “can cause disease in virtually any body compartment;” and “cause considerable mortality and morbidity rates. Exposure to one type of Enterobacter can result in neurological disorders. They do not usually cause immediate death.”
In a study looking at DNA reports of 43 root canal samples, a total of 42 different species of anaerobic bacteria were found out of a potential of 85 choices. The number of different microbes ranged from 11 to 40 in individual tooth tests. In cavitations, which are unhealed bone defects, primarily where wisdom teeth have been extracted, from 118 samples, 67 different bacteria were identified. Individual tests ranged from 19 to 53 per single sample. Again, out of a potential of 85 tested.
Staphylococcus aureus, usually reserved for hospital outbreaks, are not the most common, being in less that 23 percent of the MS, ALS, and AD samples studied, none the less can be part of the team destruction process. Aureus is noted to kill white blood cells of the immune system. Common denominator? Is it proper to have a reservoir of them with their toxins readily available for distribution each time a person bites down? The way the system operates, biting down on a root canal tooth can squirt toxins out into the system, but antibiotics and white blood cells cannot get in through the combination calcium – blood clot barrier provided by the body’s reaction to certain bacteria.
Looking briefly at the bacteria and their published toxicity for connections to these people, these bacteria became suspect: In Amyotrophic Lateral Sclerosis (Lou Gehrig’s disease, or ALS)
Evaluating 29 samples:
- Veillonella parvula 58 percent – pathology associated with heart disease and destruction of the Central Nervous System.
- Candida albicans – 65 percent – as it changes from yeast to the fungal state, it becomes invasive, causing small holes to occur in the intestinal tract resulting in “leaky gut syndrome”. Also increases porphyrin excretion in urine leading to reduced ATP and heme formation, thus reducing overall energy to cells of the nervous system. Capnocytophaga ochracea – 58 percent – can cause frontal lobe brain abscesses – associated with dental infections and diseases of the Central Nervous System
- Porphyromas gingivalis – 75 percent– alters the integrity of endothelium of blood vessels. Enhances atherosclerosis.
- Gemella morbillorum – 68 percent – noted for endovascular infections and meningitis.
Evaluation of 40 Multiple sclerosis samples in which 81 separate microbes were identified, seven are reported here.
Although not defined as a neurologic disease, draining sinuses are common among MS patients with root canals, so Actinomyces was included.
- Actinomyces naeslundii – 35 percent – associated with draining sinuses (generally clear up within a week of root canals and cavitation treatment)
- Candida albicans – 62 percent – described in ALS section.
- Capnocytophaga ochracea – 42 percent– frontal lobe brain abscesses of dental origin – microbe thought to originate in dental decay.
- Gemella morbillorum – 57 percent– associated with meningitis.
- Neisseria meningitides – 7 percent– associated with seizures.
- Escherichia coli – 12 percent- and Staph aureus – seven percent are both capable of increasing porphyrins, which will cause less ATP to be available to neural tissues.
- Streptococcus intermedius – 27 percent – Cervical spinal cord abscesses – associated with high mortality and neurologic morbidity.
Dr. Hal Huggins, had researched toxicity of dental materials for 40 years. His presentation at the Toxic Element Research Foundation covered the most influential diagnostic chemistries selected from his base of 200,000 data points.
He found that many victims of autoimmune disease showed improvements in blood chemistries discussed in his presentation that clearly indicate recovery from disease is a possibility when the challenging bacteria are removed with proper protection for the patient.
Millions of people stand to regain their lives, and countless more millions will never have to contract the diseases thought to be related to the combination of dental mercury, nickel, aluminum, root canal, and cavitation anaerobic bacteria as they combine forces to destroy the immune system.
THE “FOCUS” HAS BEEN DESCRIBED AS A CHRONIC, ABNORMAL, LOCAL change in the connective tissue, capable of producing the most varied distant effects beyond its immediate surroundings, and therefore in constant conflict with local and general defense (Pischinger and Kellner). By this definition, even a fully-healed scar may sometimes act as a focus, spreading disease to distant parts of the body. But the foci we shall now examine will be confined to those of the THEET and tonsils – in my view, the most lethal of all foci.
The emphasis I place on the REMOVAL OF DEVITALIZED TEETH and chronically – diseased tonsils in one of the better-known aspects of my work, but also one of the most criticized and misunderstood. I do not, for instance, recommend that healthy tonsils and teeth be removed from a healthy person. But I believe if they are diseased, they cause the body’s natural resistance to be lowered, thus acting as an important contributory factor to tumors development. In these cases, I insist on their REMOVAL.
It is sometimes argued that to carry out such operations on seriously ill patients is unnecessarily cruel, even irrelevant. There are some unpleasant side- effects, but in my opinion, the benefits- which I will describe- more than make up for any temporary discomfort. It is further argued that in the cancer patient, as much lymphatic tissue as possible should be preserved, and that therefore tonsillectomy should not be carried out because even a diseased tonsil may retain some useful defense potential. I used to believe this as so. I do not any longer for reasons which will become evident.
In addition, my experience shows a direct connection between dental and tonsillar foci and many of the illnesses responsible for early debilitation and untimely invalid sing.
It has long been generally accepted that head foci may give rise to almost all kinds of chronic, and certain acute diseases, such as- to mention a few- the manifold varieties of rheumatic and cardiovascular conditions. The removal of such foci is today a routine art in the conventional treatment of those diseases. However, the fact that head foci are also a contributory cause in the development of neoplasia, by lowering resistance, has received all too little acknowledgement.
The extent of the disease- provoking activity of a focus in distant parts of the body depends on whether the body is able to oppose the focus with its own defense mechanism. As long as the focal situation is kept under control by the local defense mechanism, no focus- induced remote effects will arise. On the other hand, distant effects will arise when the body’s resistance has more or less broken down: control of head foci will then gradually collapse, and there will be a consequential gradual increase in generalized focogenic intoxication. This will cause an inevitable deterioration of the body’s defense power with a concomitant promotion of malignant growth.
Nearly everybody is confronted with DENTAL PROBLEMS at some time in their life, and even the most scrupulous dental care cannot guarantee dental health. Endogenous factors, such as prenatal damage to the embryonic dental tissue, as well as exogenous influences, such as malnutrition and toxins, must essentially be held responsible for the great number of dental diseases, be they a weak, susceptible gingival, or gum; or teeth which are mal positioned, barreled or impacted; or worst of all, a disposition “to decay “.
Despite its porcelain-like surface, the crown enamel of the tooth is vulnerable to decay. Enamel defects develop especially in the grooves of the crown or on the adjacent surface of neighboring teeth which are difficult to clean.
Decay is not painful so long as it is confined to this nerveless enamel layer. The onset of a toothache is the first noticeable sign that the decay has invaded the dentine body of the tooth which, unlike the enamel, does have nerves. If this decay is allowed to continue, sooner or later the dentine will be completely penetrated, and the pulp (nerve) inside the tooth will then become inflamed.
As long as only the outer enamel and dentine are affected, the tooth can be preserved. But a tooth with an inflamed pulp ca no longer be saved, and must be extracted without delay.
In an understandable desire to preserve as many teeth as possible, to maintain the masticator apparatus and its functions, attempts are often made to save teeth which are in fact lost. There is a widespread conviction that this can be done without risk by the sterile evacuation of the pulp, and then refilling the cavity. For decades, the erroneous belief was held that, after such treatment, the tooth is an isolated, lifeless thing, no longer involved in any of the body’s processes. This assumption was originally based on the premise that the pulp cavity had only one orifice to the apex of the root below, and by filling, this opening was sealed. However, the dentinal canal does not end in just one opening; instead, it resembles a tree with many branches which penetrate the tooth’s body in all directions.
The finer details of the entire dental structure have been exhaustively studied by Austrian researches. They have established that there is a lively metabolic interchange between the interior and exterior milieu of the tooth, and that this two- way process takes place along many thousands of hyperfine, capillary canals joining the pulp cavity to the exterior surface of the tooth. Very careful conservation measures may possibly seal of the vertical central-medial-tube of the dentinal canal, but, it will never reach the lateral “twigs” branching off from this tube. Nor can it ever close off the innumerable capillary canals. Some protein will always remain in these secondary spaces. If this protein becomes infected, toxic catabolic products will be produced, and conveyed into the organism.
It was established in 1960 by W. Meyer (Gottingen) that within devitalized teeth the dentinal canals and dental capillaries contain large microbial colonies. The toxins produced by these microbes in a tooth with a root filling can no longer be evacuated into the mouth, but must be drained away through the cross- connections and unsealed branches of the dentinal and capillary canals into the marrow of the jawbone. From there, they are conveyed to the tonsils, and thus the flow systems of the body. In fact, the conservation treatment may literally convert a tooth into a toxin producing “factory”.
A devitalized tooth is no longer able to perceive and control inflammatory processes even when suppuration has invaded the surrounding bone spaces of the tooth’s socket; it rarely gives warning signals, for instance through pain, and therefore there is nothing to induce the patient to have this dangerous toxic focus removed. It then may be left to develop its devastating effect on the organism for decades or even for a lifetime.
When the inflammation spreads to the marrow of the tooth socket, it can cause Osteomyelitis. Its further course is determined by whether and for how long the local defense is able to keep the focal disturbance under control.
If the body’s local resistance is intact, the inflammation is enclosed by a capsule of connective tissue known as the DENTAL GRANULOMA. This membranous cyst prevents its toxic from spreading into the organism. Radiographs of these teeth show granuloma cysts as more or less marked transparencies, showing a darker irregular radiolucent area on the apex of the root. This type of tooth is called X- Ray positive.
If the body’s local resistance is weakened to such an extent that the inflammatory process cannot be encapsulated by the granuloma cyst, the toxins will be able to advance unhindered into the marrow space, the tonsils, and into the body. In this case, it is proof that, as stressed by Pischinger and Kellner – the organism has become largely incapable of reaction. Radiographs of these teeth as a rule show no transparencies, and are therefore called X- Ray negative.
In my cancer patients, I have found that such non –encapsulated foci- that is those who show X-ray negative- were particularly common, as one would expect from people whose body resistance had been lowered.
Today there is general agreement that dental foci should be cleared away, and it has become usual to diagnose them by X.-ray.;’. Unfortunately, only some of the dental foci ca be discovered by this means. Encapsulated foci can be recognized only if large enough, and if not concealed by the tooth’s shadow. And definite X-ray signs are much rarer in non-encapsulated Osteomyelitic processes. It is therefore the most dangerous of all dental foci which most frequently prove X-ray negative. Even with X-ray positive dental film only those foci can be recognized which happen to be situated outside shadows. In X-ray negative foci often escape treatment- and they are the ones the body has failed to resist effectively – the can continue to develop their destructive effects unhindered.
My clinical experience has produced evidence of a causal connection between foci and tumor development, and in this respect, the results obtained with the aid of an infra- red test are especially significant Any inflammatory disease focus creates on its corresponding skin surface a pathological increase of infra- red emission; the higher the activity of the focus, the more pronounced it is. Using an infra- red sensitive instrument (Schwamm’s infra-red toposcope) the intensity of this emission ca be continuously monitored and measured. Observation showed a close interrelation between the infra-red emission of head foci and that of the neoplasial region. That is, after treatment, a decrease in the infra- red activity of dental foci was as a rule accompanied by a decrease in infra- red emission over the tumor areas.
From this it is clear that the advisable treatment for devitalized teeth is SURGICALLY EXTRACTION.
But even this is not always enough. My experience has further shown that also living teeth may sometimes be so damaged that their pathogenic potential almost equals that of devitalizes teeth. For instance, latent chronic pulpitis (pulp inflammation) may arise in a tooth that appears out –wordily healthy, thus having a focal effect.
The diagnosis and treatment of dental foci remains generally unsatisfactory. A survey conducted at my clinic found that, on admission, ninety- eight percent of the adult cancer patients had between two and ten dead teeth, each one a dangerous toxin producing “factory” Very often we are confronted with X- ray, negative dead teeth, root remnants, and residual osteitis (Cavitational Lesion ‘NICO’) which had not been diagnosed and therefore had not been removed.
Only total, thorough dental treatment will really succeed in giving the body’s defense a chance. In addition to X-ray diagnosis, it is therefore necessary to use other diagnostic aids. Such as infra-red techniques tests, to estimate tooth vitality and periosteal resistance, and other electrometric methods.
The diagnosis of foci in teeth has been greatly improved by electro acupuncture, is now possible to differentiate foci not only with regard to their type and position, but also to their virulence and pathogenic efficacy. The result of focus treatment can consequently be observed and improved, before, during, and after dentistry, to an extent never known before (Kramer).
If total treatment is to be performed, it is necessary to remove not only any devitalized teeth but also any hidden dental foci remaining in the jaw. Further, total removal of devitalized teeth and their roots must not be the end of the dentist’s activities. Each alveolus, – the tooth’s socket in the jaw-should be radically cleared down to the healthy bone. In that way the development of a residual osteitis (Cavitational Lesion “NICO”) or of a cystoma may be prevented. It Is not only the tooth which may be a focus, but the adjacent tooth –fixing apparatus as well. There are four different ways by which dental foci – and indeed all foci- can affect the organism and contribute to the development of secondary damages:
- The “neural” way of affecting the organism. When a focus develops anywhere in the transit tissues, the mesenchyme, the process is centripetally projected from the terminal neural organs around the irritated area, along the neural ducts, up to the corresponding control cells within the central nervous system. The irritation origination from a focus ca, under certain conditions, trigger of the mechanism of a neural dystrophy a slow degeneration which my show itself in localized effects in other areas, but also in a generalized dystrophy disturbance. In the 1950 it was shown that these manifestations are based on depolarizing processes in the effected neural cells, and in the corresponding tissues of the body’s periphery. (Fleckenstein and Ernsthausen) By elimination of the focus, the affected tissues may be repolarized. The most striking example of this repolarization is called “second-phenomenon”. Ferdinand Huneke, the founder of neural therapy whose remarkable contribution in this regard we shall look at in detail later, discovered over forty years ago that injection of a local anesthetic near a primary focus may immediately remove any symptoms of distant disease induce by the focus. This effect – the second-phenomenon –usually takes place only in those a few seconds after the anesthetic injection and lasts for hours, days, or even for a life time. Naturally the improvements occurs only in those regions influence by the injected focus. Nevertheless, the measure has therefore a remarkable diagnostic value as well. Since neural therapy only neutralizes the neural effect of a focus, the focus itself must, of course, be removed after such treatment, in order to eliminate its latent toxic or allergenetic action. Conversely, any focal surgery must be followed by desensitizing and neural-therapeutic measures. The only exceptions to this rule are, for instance, featureless scars of other spots with no inflammatory change which produce only neural distant effects without at the same time causing any toxic, microbial or allergic secondary phenomena.
- The “toxic way” of affecting the organism. The toxic activity of odontogenic foci is probable far more perilous for the organism than their neural effects. The mechanism of this distant toxic activity, as well as the characteristics of e toxic compounds involved have been largely ascertained. Odontogenic compounds are the gangrenous contents of an inflamed. Commonly found in tissues destroyed by inflammation, liquefaction and microbial putrefaction. Thus, there ca be little doubt that they are genuine necrogenous toxins, including for instance autologous protein and higher- molecular proteinogenous compounds. 3Later there will be produced numerous low-molecular fission products resulting from enzyme cleavage and other biogenic conversions. The identity and chemical structure of certain of the biogenic amines were mainly clarified in the 1950 by Schug-Koesteris, Hiller, Gaebelein, and others of the University of Munich. Following similar findings in America, the metabolic and exchange processes in solid dental structures were further investigated by the German researcher Spreter von Kreudenstein. He showed that drugs injected intravenously were, four to five hours later, discernible within the intra dental capillary ducts or even devitalized teeth, and in a concentration only slightly lower than in the blood. All these findings prove conclusively that within solid dental structures, there may proceed an unimpeded substantial interchange in either direction. Consequently, odontogenic toxins, wherever they may have been produced, are able to diffuse and circulate within the organism. The pathogenic significance of these, “endotoxins” has been investigated by the German study group of Eger-Miehlke. They examined the changes in healthy experimental animals after injection of accurately defined, minimal quantities of the endotoxins from an “Odontogenous Granuloma”. A single injection of a minimal dose seemed to develop a defense activating effects. But after repeated injections, there was severe liver damage, and the animal died within weeks. Apart from the fatal liver damage, inflammatory and degenerative changes were found in all other organs, especially in the joints, muscles, and blood vessels. These results brought clear experimental proof for the first time that focogenic toxins act as causal agents for severe diseases in animals corresponding to similar chronic conditions in man. The most dangerous of all odontogenous toxins are undoubtedly the thio-ethers, for instance dimethylsulfide. In a series of test performed at my clinic, it was observed that patients with odontogenous and tonsillar foci had a heightened level of dimethylsulfide in their blood. After intensive treatment of the foci, this level returned to normal in just a few days.Thio-ethers are closely related, both in their structure and their effect, to mustard gas and other poison gases used in the First World War. The extreme toxicity of the poison gases and thio-ethers can be attributed to the following properties:
- They are weakly basic, therefore “electro-negative” and thus they are deposited particularly in “electro-positive” cells such as those of the transit tissues as well as those of the defensive tissues.
- They are soluble in the lipids, and therefore have a pronounced tendency to enrich themselves in the lipoid- containing cellular structures, especially in mitochondria.
- These subcellular organelles, attached to their lipoid membranes, contain the enzymatic structures responsible for the maintenance of aerobic metabolism a precondition for full functioning power in all the body’s cells and tissues. If these indispensable units are damaged the most serious consequences will follow. Because they are the most vulnerable cellular organelles, mitochondria are a favorite and almost exclusive target for thio- ethers.The action of thio- ethers is affected in three main ways:
- Since thio- ethers tend to combine with electro- positive metal ions and many bio-elements which act as co-effectors or activators of numerous enzymes ob absolutely vital importance, and as our present-day average diet is deficient in essential substrates such as vitamins and bio-metals, this deficiency is enhanced. Much of the daily intake of bio-metals, usually deposited in the fluids of a focally affected organism. Will be made permanently ineffective, the more foci the greater will become the deficiency.
- Thio-ethers are “partial” antigens, haptens, and thus they also tend to combine with the normal proteins in the body, “denaturizing” them. Such denatured proteins become “non-self” agents which the body must deal with as such. The production of antibodies adapted to the situation will be provoked, and they will home in on the target antigens wherever they are. The process of “auto-aggression” will be set in motion: self-destruction of agent’s alien to the organism. Extensive structural cellular damage will result, increasing with age.
- The famous biologist, Otto Warburg, twice winner of the Nobel Prize, has shown that aerobically – blocked cells – as caused by thio-ethers- will increase their anaerobic metabolism in an attempt to maintain their vigor. In doing so, they acquire the characteristics of malignant cells. Therefore, chemical agents capable of inactivating the aerobic process while increasing the anaerobic process are usually classed as carcinogenous compounds.
Druckrey (Heidelberg) found inter alia that transformation of a normal cell into a malignant cell requires a certain quantity of a carcinogen – the carcinogenic minimum dose. It does not matter whether this quantity is supplied in a single dose or in a number of smaller doses, because the toxic effects of each dose are stored, and accumulate without loss. The carcinogens held primarily responsible for the development of spontaneous cancer in man are those: which inhibit the aerobics even in minimal quantities without at the same time immediately destroying the cell, and which are constantly present in the organism in this minimal concentration of either endogenous or exogenous origin; they can therefore accumulate during the normal life expectancy gradually and unnoticeably until the total quantity necessary for maligners is reached. There is hardly a carcinogen which so completely fulfils these conditions as do thio- ethers. Incessantly, from the moment the pulp is removed, hour by hour, year by year, minimal amounts of these most virulent of all the odontogenous toxins will be released into the circulation –minimal doses, but nevertheless sufficient to more or less totally paralyze the aerobic action of the cell. The nervous system is thus doubly affected by focal intoxication.
Intoxication of neural cells caused by the toxins spreading through the liquid vehicles of the flow systems, such as the blood and lymph. The more mitochondria a cell contains, the more it will be damaged by the enzyme- inhibiting effect of thio-ether compounds. Therefore, it is the vital organs, the liver, nervous system, endocrine glands, heart, and reticuloendothelial system – whose cells my consist of up to one-fifth of mitochondria, that are primarily affected. Apart from disturbing regulatory control, odontogenous toxins will also cause additional damage almost throughout the body. Naturally, the higher the blood- level of foco genous toxins, the more severe will be their effect.
The close interlacing of the lymphatic and endocrine systems in the head, make it unavoidable that brain cells are more intensively toxicities by the circulating focogenous agents and may suffer particularly heavy damage. The lymph ducts of the had region join Waldeyer’s tonsil ring where detoxification takes place. There, inflammatory swellings inevitable cause a lymphatic congestion. All the toxic sewage of head foci are channeled into Waldeyer’s tonsil ring, and if there is such congestion, waste fluids will be pressed through the porous base of the skull into the lymphatic space of the brain. Toxogenous changes, especially within autonomic nuclei, are regularly found in cancer patients. As verified in the q930 by Muehlmann (Moscow) and they may be a consequence of a life-long inhibition of cerebral aerobics due to focogenous intoxication. The cerebral damage (diencephalosis ) and the subsequent loss of vitality in cancer patients is accompanied by a number of other symptoms. The emission of hypothalamic energy impulses, recordable by a Voll’s electro- acupuncture device, are reduced in patients with focal disease. The autonomic vigor is relaxed, creating “regulation rigidity” carcinomas tend to parasympathicotonic derailment; in sarcomas and systemic diseases, as a rule the opposite is found- sympathicotonic derailment (Regelsberger, Gratzl-Martin, Rilling et al) The diurnal, circadian regulation of the acid-base balance is lost ( Sander) . At the same time, there will exist a distinct inhibition of other diurnal control functions, for instance of blood sugar, cholesterol, and mineral metabolism, and many other metabolic parameters are greatly restricted (Hinsberg).
- The “allergic” way of affecting the organism. The toxic effects of thio-ethers (Root Canal and Cavitatrional lesions) overlap those caused by higher- molecular odontogenous toxins, as already described. Antibodies are formed to fight these substances, eventually leading to the destructive processes in toxified cells. Since the organ- destroying antibodies or defense enzymes are excreted by the kidneys, they can be diagnosed in the urine by the Abderhalden test. In this way we can precisely deduce, in most cases, which organs have suffered secondary damage (Abderhalden, Dyckerhoff et al). The extent of secondary lesions can also be demonstrated indirectly by vaccine treatment. Using desensitizing vaccines made from focogenous agents, reactions are caused in regions affected by distant focal effects which may become evident in regional as well as general symptoms. It is thus clear that the development of cancer disease, is in more ways than one, closely linked with focal events.
- The “Bacterial” way of affection the organism. Bacterial dissemination from primary “Dental Foci” as a rule takes place with barely perceptible symptoms, and may be followed by the formation of “Secondary Foci” in other regions. These include, inter alia, Foci in the Paranasal sinuses, gall- bladder, appendix, prostate and renal pelvis. Above all, bacterial dissemination tends to produce micro foci or micro thrombi in veins, and they in turn have a tendency to thrombosis or thrombus phlebitis, possibly with concomitant embolism. Thrombus phlebitis and thrombosis, so common in cancer patients, and generally regarded as resulting from disordered metabolism, are due not only to the dyscrasia of those patients, but also to the manifold effects of “Dental Foci “. We have now seen how decisively the entire organism is affected by “Dental Foci” not properly treated, and what catastrophic results destruction of the pulp may entail. Dentists must, therefore bear in mind that there is no root treatment which does not inevitably produce foci. The dentist’s task is l only secondarily cosmetic; primarily it must be preventive and curative. The over- riding consideration must not be conservation of the tooth but preservation of its vitality. If this is impossible, even the most beautiful crown must not delude us that the lifeless tooth beneath is anything other than a “corpse in a golden coffin” whose decomposition toxins slowly but surely are destroying the organism (Bircher-Benner). Other foci in the jaw, for instance Cavitational Lesion Osteitis Residual, Osteitis, cysts, foreign bodies, gingivitis, and malposition of teeth may also develop focal effects. It goes without saying that these foci, disturbance fields and centers of irritation must be removed. The dentist should always remember that he has a vital role to prevent the development of chronic illness and, most important of all to decisively reduce the hazard of cancer.
Additionally, this information begs these questions to be answered:
Should the public be informed about the potential real danger of toxins from root canals and cavitations, regardless of the consequences, financial and otherwise, to the ADA and dentists?
And what will patients, government agencies, and the dental profession do about this?

